
Posted by: The Sumaira Foundation in NMO, Patient.e, Voices of NMO
 My name is Letitia and I am a 22-year-old South African NMO patient. My story began on the 26th of December 2017, Boxing Day…
My name is Letitia and I am a 22-year-old South African NMO patient. My story began on the 26th of December 2017, Boxing Day…I had been suffering with an excruciating headache for the last 2 days. I eventually noticed that I also had trouble with my peripheral vision. After some online research, I came to the conclusion that it was most likely a tension headache, and that once the headache was gone, my vision would likely be restored. In the interim, however, I had taken to wearing sunglasses in an effort to keep out any light as it appeared to intensify the pain.
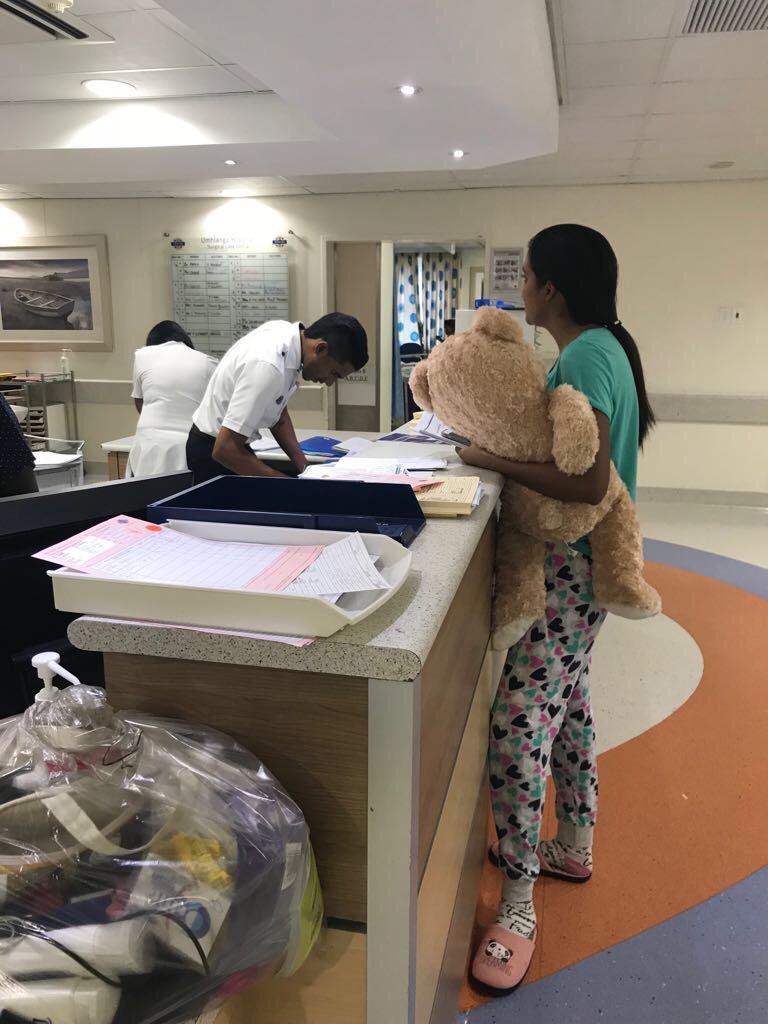
I was on holiday in my hometown, Durban, South Africa, where our family doctor was on leave for the festive season, so my only option was to treat the headache with over-the-counter pain medication, which proved to be ineffective. I laid in bed most of the day with a beanie over my eyes, desperately trying to block out any light and help with the photosensitivity. Later that evening, I was taken to the hospital as my symptoms got worse.
I remember laying in the hospital bed at the outpatient department as they checked my temperature and shone a light in my eyes to check them. “They’re normal” the nurse kept saying, and I wondered how my eyes could be normal if I could barely see? I was given a paracetamol drip which helped the pain a little and the on-call doctor ran several tests for things like meningitis, malaria, etc. After some time, the nurse stood in front of me with the thick pile of test results in her hands telling me that they came back normal, to which I responded that I still could not see.

After spending my very first night in hospital (not knowing that it would be the first of many), a physician examined me and concluded that my symptoms were that of a typical migraine but because I had never had a migraine before, I was sent for my first ever brain MRI as a precaution.
This was how my journey started at the age of 20. After the results of that first MRI showed an infection in my right temporal lobe (right temporal encephalitis), I spent 3 weeks in the hospital being treated with acyclovir for herpes simplex encephalitis (HSE), which is what my neurologist thought was the cause of the brain infection. The pain began to subside and after a visit to the ophthalmologist showed optic nerve damage and inflammation, I was given occupational therapy which helped to slowly regain my peripheral vision. I was discharged mid-January with a follow up appointment scheduled for the end of February, just a little over a month later.
I never actually made it to that appointment, instead I spent the next few months in and out of hospital. First, because I was off balance and couldn’t walk without tilting to the side, supposedly caused by a middle ear infection. Second, due to severe vertigo, I couldn’t even turn my head without vomiting and losing bowel and bladder control. I lost 6 kgs in 4 days.
After a consultation with a gastroenterology doctor and a gastroscope to accompany it, a stomach ulcer due to the medications was supposedly the culprit. After this, I had been in for checkups with a neurologist occasionally, but it was upon my third stay, 2 weeks later when everyone involved started taking things more seriously.
I could hardly walk or see properly and my eyes were jumping from left to right, unable to focus on anything. My balance and equilibrium were completely off and so everything I saw and felt was tilted. I lost my appetite and experienced numbness in my tongue which effected my speech. A brain MRI showed severe cerebellum infections and so I began steroid treatments both orally and intravenously.
We sought the help of several neurologists, neurosurgeons and professors of neurology for answers. The best they could do was treat me for diseases such as tuberculosis, listeriosis, Cat scratch disease etc. as they were not certain what was causing the reoccurring brain infections. During this time, simple tasks such as taking a shower, sitting upright, walking, and even using my hands were difficult and physically draining. I napped most of the day but could never sleep off the pain or exhaustion. Countless MRI’s, lumbar punctures, blood and other lab tests were done to help find a diagnosis. At this point, my neurologists tried and failed to find answers as to what this could be until April 2018.
I had just been discharged after an MRI and lumbar puncture, so when I started experiencing sharp pains in my back and couldn’t sit up straight, I thought it might just be a side effect of the lumbar puncture. Then, came a painful burning sensation around my waist and numbness in my feet. An MRI of my spine showed a lesion in the T10 region. This is when we first started hearing of a rare disease called NMO, and so the testing began. The AQP4 and MOG tests had come back negative, however, my story comes with a twist…
My neurologist sent me for thyroid tests as precaution because at that point, we had done so many tests except that one. This is how we found out that I had a cold nodule on my thyroid. I underwent a right thyroid lobectomy and the nodule was removed and tested. The tests came back positive for cancer and 75% of the tumor cells tested positive for AQP4 which led the doctors to conclude that the cancer had caused the NMO – Paraneoplastic syndrome thyroid carcinoma.
Since then, I have had 4 Rituximab Infusions (2 full doses). I’ve been on high doses of prednisone which came with a variety of side effects, both physical and emotional. In 2018, I had gained 16 kgs over the space of a few months, leaving me with 3 chins and a moonface. In 2019, I was diagnosed with depression and put on anti-depressants and anti-anxiety medications for a few months. This was a result of chemical imbalances resulting from the brain infections, the mix of medications I had been on, as well as preexisting issues with depression. I found that the medication wasn’t the right method of treatment for me and so I sought other ways to maintain better emotional and mental health.
Because of a lack of data on rare cases like mine, my doctors still do not know whether removing the tumor means that the NMO is gone for good or whether a relapse awaits me.
This has been a long, emotionally and physically draining experience and I’d be lying if I said that all this uncertainty doesn’t get me down, but thankfully over these past two years, I have developed coping mechanisms which are healthy for my mind and body. I still have bad days where I am unable to walk properly and the chronic pain intensifies, but I also have really good days, filled with high energy levels and gym classes, so I have learned to just take each day as it comes!
I wouldn’t have gotten through these dark times without my family, friends, doctors and my fellow NMO and cancer survivors; I’m so grateful for all their endless support. I am determined to use this experience and my story to help others and hopefully raise NMO and rare, chronic illness awareness so that anyone going through similar experiences never has to feel as alone as I felt in the beginning of my journey.
If you or someone you know is fighting a similar battle here are a few things to keep in mind:
